18 Jan The three Rs!
Patients usually come to see us here at Openhealth because they’re in pain. Our job as therapists is to understand the root cause of that pain, so we can devise the best possible treatment and management. This starts with a good case history, hence us always taking the time to speak to our patients. In fact, amongst the medical profession, it is thought that 80% of a good diagnosis comes from the case history – that is before any examination or testing.
The usual starting point is knowing where the pain is. This might sound obvious, but there’s more to formulating a diagnosis than just letting the patient point to it, and allowing us to prod it! If you can pinpoint your pain, we might be able to identify a particular joint, tendon, ligament or muscle that’s responsible.
But if the pain is more diffuse or the mechanism of injury less obvious, then we probably need to know more… We might ask questions such as “what movements hurt?” or “when do you get the pain during the day?”. As this information is gathered, an experienced practitioner might recognise particular patterns of pain.
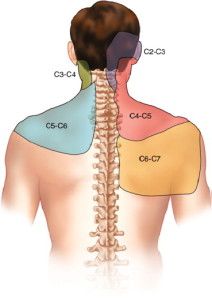
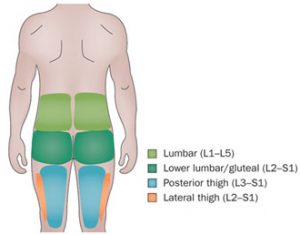
For example, if a patient has irritated a joint in their lumbar spine either in sport or heavy lifting they often feel dull pain through their low back and into the buttocks and thigh as well as some pinpoint pain. We call this spread of pain a RADIATION since the problem is in the joint, but the nervous system is getting confused and reporting pain elsewhere as well. The patterns have been researched using (brave) volunteers who had their joints injected with saline to make them swell before reporting where they felt pain.
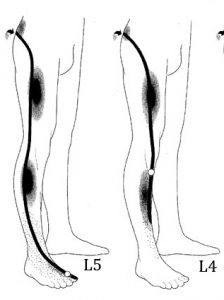
Nerve root pain can be very sharp and cause other symptoms. The patterns are relatively easily recognisable
If on the other hand you have done something to your low back that has irritated a nerve that runs to your leg you may feel symptoms throughout the whole nerve, ie down to the foot. Patients commonly get pins and needles, numbness, and maybe even weakness. The pain can even be so bad that patients are relatively unaware of their low back. This is called a RADICULOPATHY, and when it affects the sciatic nerve is called sciatica. It can be quite serious, but is relatively easy to test for, and often responds very well to manual therapy (if it’s not too acute) and good advice regarding activity, medication and self-help.
Lastly, we have REFERRALS, which take us more into the world of medicine. Why does this matter? Well, if you’re feeling pain in your left arm, we need to make sure this is not coming from your heart!

The gall bladder causes pain locally (dark pink), but is also known to send pain to the right shoulder
One of the reasons it takes so long to train as an osteopath or physiotherapist is because we have to learn to recognise the difference between mechanical issues and signs of an illness or disease to make sure we treat the patients we can help, or refer those we can’t to the proper person. So when we ask about shortness of breath, chest pain, or any changes to digestion or urination, it’s because we’re making sure you’re in the right place!
So next time you visit one of us and we seem to be asking a lot of questions, it’s probably because we’re sifting through the evidence to help us work out what’s wrong with you! When we examine you, we hope to be confirming our hypothesis, and not just poking you until you say “Ow!”
If you’re reading this article and have any worries about your own health or the pain you’re in, then get in touch with us and one of our practitioners will be happy to help you.



No Comments