
12 Jun Low Back Pain – Four Points to Consider
Research around low back pain is changing. It’s no longer all about treatment techniques or new exercises but rather explores what we know about patients suffering from persistent back pain, and how they interact with the world around them. We thought it would be useful to go through some of the salient points. Here goes!
Point One – It’s about behaviour and fear, not damage!
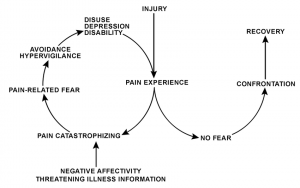
Most cases of disabling low back pain begin with some genuine damage, but this heals up. However, patients are left fearful of re-injury. This is not entirely inappropriate, but what happens in some cases is that the fear takes over. This leads patients to avoid doing what they used to do, makes the pain worse, and a vicious circle is formed. Pain leads to less activity, and less activity leads to pain.
If we want to understand why this happens to some people and not others, we have to look at their environment and what they understand about their original back pain. Too often, we meet patients who have been told:
- that their spine is fragile (it very rarely is)
- that certain movements should be avoided (they almost certainly shouldn’t, at least not in the long term)
- that there is a long list of damage in their spine (there is in everyone’s spine if you look closely enough!)
The result is that patients develop an overwhelming fear response when judging the risk of performing a particular movement. They then decide not to do it. Sadly, it doesn’t take too long before a patient’s distrust of their body becomes more and more disabling.
Therefore, we as a profession are starting to understand more clearly that the route to recovery should not rely on passive treatment (when someone else is doing massage, manipulation or acupuncture).
Instead, a patient’s recovery should include some form of exercise or movement therapy. This way, patients can explore how their body feels as they move. With education and reassurance, they can hopefully find natural, pain-free movements, even if very limited. From that starting point, they can begin to build trust and confidence.
Point Two – Relaxation might be more useful than Strength for low back pain!
As soon as patients hear the words “exercise” or “rehab” related to low back pain, they presume that they need to strengthen their core and walk around with rigid tummies. Wrong!
It’s all about having a variety of movement strategies in order to carry out the range of activities we ask of our bodies. Some of these need tension, others don’t. (You can read more about this in our Core Blimey blog).
One of the times we do rely on some more tension in our body is when we’re experiencing acute pain. At these times, it’s more than appropriate to brace ourselves to limit spinal movement, but as our tissues recover – which might take up to 12 weeks – the need for such a strategy fades away. However, problems arise when a bracing strategy lingers on, making people stiff.
We regularly see such behaviour in patients who describe a fear of “letting their core go”, or who look to be suffering from a recent injury only to tell us that they’ve been struggling with it for 6 months or more!
What is effective with these patients is to educate and reassure them and teach them to relax their spines again in a way that feels comfortable and allows them to develop trust in their joints and muscles again.
This rehab is less tortuous compared to what most people expect! Breathing exercises can be used to calm the body’s overall reaction to pain, and then patients can learn to relax the spine and move it gently.
Part Three – The Mind Matters…
We’ve mentioned education and reassurance already, and these are effective forms of treatment as they tackle the patient’s psychology. Manual therapists are by no means psychologists, but by talking with patients we can find out how they feel about their body:
- We know from research that having a negative outlook about your physical condition increases your pain experience, so if we can do anything to change this, it will help.
- Similarly, the memory of past pain can amplify any discomfort,
- The same goes for listening to the experiences of family, friends and colleagues – despite those people’s best intentions!
Instead of giving instructions and orders, a therapist should journey together with their patient, questioning how they feel and think about their pain.
Part Four – Lifestyle Matters Too!
When researchers look at factors associated with low back pain, they struggle to find many really strong associations, despite the messages peddled by the media and certain industries.
Poor posture does not cause low back pain on its own, nor does carrying a heavy school bag or looking at a phone or book. One thing that does seem to have a strong correlation, however, is sleep.
Those who sleep badly are more likely to develop low back pain, and those with low back pain are more likely to develop sleep problems. Talk about a vicious circle! Not to mention the fact that poor sleep causes other psychological disturbances that can hamper those with persistent back and who are already struggling!
We typically tell our patients to care more about the quality of the sleep than trying to choose a position that might help their tissue recovery. They might have a rubbish night’s sleep and that causes more harm!
As for different forms of exercise or sport, there is nothing that stands out as being particularly helpful for low back pain. Some patients cope well by just walking the dog, some do Pilates, some go running.
There is, however, a U-shaped relationship between physical activity and disabling low back pain. So, if you do either absolutely no exercise or shedloads of it, your chances of developing low back pain rise. If, however you sit in the middle, then you’re less at risk.
What we must all remember is that it’s a waste of time to look for one recipe that fits everyone. We all have different bodies, different lifestyles and different environments.
Embrace the differences, and try things until you find what works, and hopefully, something you enjoy as well!
In Conclusion
Whilst we see plenty of patients with relatively simple injuries that respond to particular treatments, the truth is that back pain becomes a much more complex beast as it drags on.
Therefore, we at OpenHealth choose to broaden our scope in choosing how to tackle low back pain. Instead of ticking boxes over and over again, working to routines and telling patients what to do next, we work with our patients by sharing their journey and helping them understand how the world they live in affects their condition.
If this article has been of interest to you and you think that your condition has taken over, we are here to help. Simply call the clinic on 01344 625475 to begin your journey.
Reference: O’Sullivan et al (2018), Cognitive Functional Therapy: An Integrated Behavioural Approach for the Targeted Management of Disabling Low Back Pain, Physical Therapy, 98 (5), pp. 408-423. Available here: https://academic.oup.com/ptj/article/98/5/408/4925487
Toby is an osteopath at OpenHealth, and regularly contributes to our blogs.





Sorry, the comment form is closed at this time.